Interdisciplinary Case Report
Anthony Ramirez, DDS, MAGD
e.max Completes This Dream
I incorporated the surgical phase of implant dentistry over a decade ago with my investment of an in-office Cone Beam imaging system and becoming proficient in computer assisted implantology. Implant dentistry is an all-encompassing discipline that requires expertise in maxillofacial radiology and anatomy, Cone Beam CT interpretation, oral surgery, periodontal regeneration, advanced digital implant planning and prosthodontics, both removable and fixed. Without this additional skill set and post graduate training I simply could not deliver the results that my patients deserve. Couple this with the in-office technologies of CEREC® Primescan and CBCT allowed us to gain control of the technical processes necessary to manage and produce the surgical and restorative phases of treatment at one location.
The following will describe a case that required multiple dental disciplines to replace missing maxillary lateral incisors with fixed tooth replacements. This case is emblematic of how being able to control the surgical and restorative processes within a digital workflow can raise the level of how we practice dentistry. We need to recognize how clinical dentistry has become intertwined with digital technologies to synergistically assist us in providing enhanced diagnosis with safe and predictable treatment outcomes. A healthy 46-year-old patient who has lived for over 30 years with missing bilateral maxillary incisors desired a fixed solution to his problem. He dreamed of the day when he no longer had to look in the mirror and see his missing lateral incisors. The existing acrylic partial denture replacing these incisors along with missing upper right molars and premolars was a poor compromise at best that was becoming increasingly difficult to tolerate. He was ready for a change and was mentally, and financially prepared for what would become a life changing experience.
Our first visit included a clinical assessment of the existing maxillofacial anatomy and an advanced radiographic evaluation employing 3D imaging. Intra-oral photographs were taken and after reviewing his medical history we discussed his desires for a fixed replacement of these teeth. His recollection as to how he lost these teeth was that after five years of difficult orthodontic therapy they simply fell out. The patient was only interested in replacing the missing lateral incisors at this time and would be satisfied with a unilateral flexi partial replacing # 2, 3 and 4. Various options were communicated for the posterior teeth which could be considered in the future. He presented with a high smile line and desired fixed natural appearing teeth. Restoring a high esthetic risk patient can be our most challenging anterior case type. A dynamic smile assessment revealed a full display of this patients’ dentition which exposed anywhere from 3-5mm of gingival tissue with a thick biotype. I diagnosed this case to be complex, requiring extensive bone regeneration, possibly with multiple grafts and informed this patient of the risks, timeline and complexity of his case. Being able to communicate our patient's problems in the third dimension always breaks down barriers to case acceptance as the information gleaned via a CT scan is invaluable for both planning and educating the patient. Only with a full understanding of the challenges associated with these complex cases can a viable solution be planned and executed to our satisfaction.
Co-Discovery and Informed Consent
The treatment plan was developed and presented during our first visit, a direct benefit of having these digital technologies at our fingertips. After reviewing his 3D imaging, it was apparent that we needed to begin his therapy by augmenting the severely deficient bilateral alveolar ridge sites. The existing removable partial denture would serve as a provisional prosthesis while the grafts mature. These cases can be treated in a variety of ways including using block graft, particulate layered composite bone grafting techniques and or ridge splitting. The gingival tissue was thick, keratinized and both sites were devoid of infection which would preclude the need for any adjunctive subepithelial connective tissue grafting. Thick keratinized tissue is required to prevent gingival marginal changes that may occur after implant placement due to thin tissue. The existing alveolar bone volume decreased as we tracked the bone from the crest to its apical termination but appeared to be amenable for regeneration. The goal was to replace these two missing lateral incisors with fixed, esthetic and fully functioning tooth replacements. Without the integrated workflow this process can become disjointed and not as streamlined when working the analog world and with multiple clinicians. These methods also reduce the number of visits necessary to restore our implants by controlling abutment design and tooth morphology with in-office technology. We reviewed the 3D images together and discussed the risks associated with his case. The possible complications were communicated so that the patient could make an informed decision and proceed with treatment. (figs. 1-3)

Figure 1: Initial presentation of missing teeth #7 and 10

Figure 2: Close up views edentulous sites #7 and 10
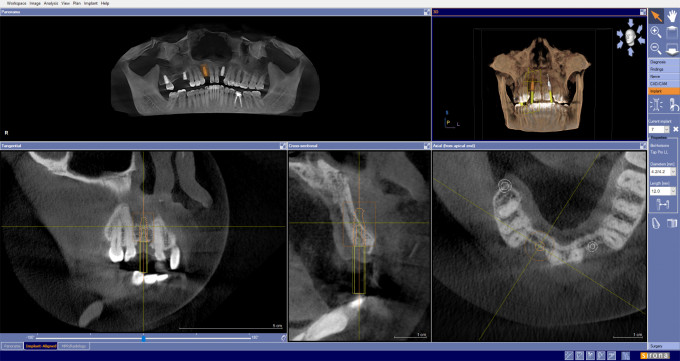
Figure 3: Pre-op CBCT imaging and virtual implant #7 with deficient bone site
Regenerating Bone Volume
The patient presented for his first surgical appointment premedicated with Amoxicillin 500 mg. Three carpules of 4% Articaine with 1/100,00 epinephrine was administered producing profound anesthesia which lasted throughout this visit. I chose to regenerate these sites with buccal bone grafts, using MinerOss Blend, a 50/50 mixture of cortical and cancellous mineralized bone allograft. Full thickness flaps exposed the underlying boney defects, and the alveolar bone was prepared with intermedullary bone preparations (decorticated) to initiate bleeding bone. Angiogenesis connects the existing tissue with the bone grafts and carry the cells and growth factors to the sites necessary to accelerate bone growth leading to regeneration. I utilized 2CC of the mineralized freeze-dried allograft, particle size 500um to 1000um. The bone grafts were covered with Bio-Gide non-cross linked collagen membranes using a double membrane technique and the areas were sutured with primary closure. I modified his acrylic partial to avoid contacting the surgical sites. The patient tolerated this surgery well and was dismissed with post-op instructions to continue antibiotic therapy for five days, 1 tablet tid and rinsing twice a day with .12% chlorhexidine. Ibuprofen 600mg was prescribed to be taken one tablet every 8 hours as needed for pain. I followed this patient closely for three months and healing was uneventful. (figs. 4-5)
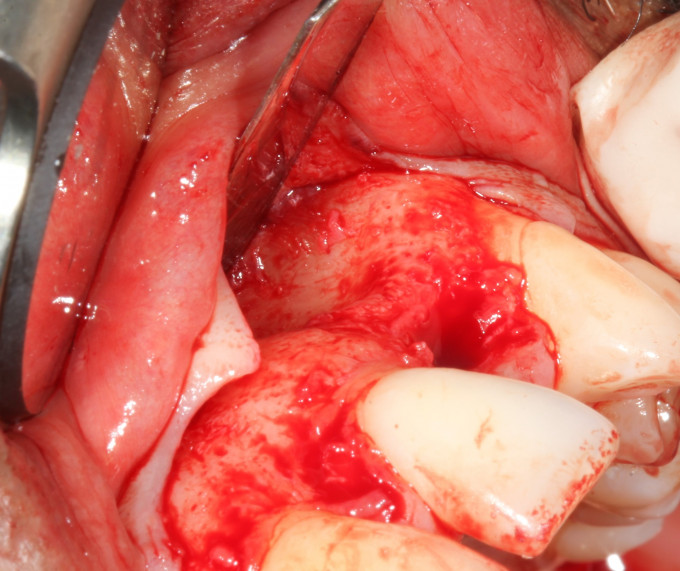
Figure 4: Exposed bone defect site #10

Figure 5: Bone regeneration surgery completed
Integrating Technologies for Implant Planning
I obtained a Cone Beam CT scan after 12 weeks to evaluate the result of his bone grafts and began digital implant planning. The Dicom file was loaded into Simplant software and virtual teeth were placed to help formulate a prosthetically driven implant plan. 3D imaging is helpful to produce the proper 3D position for the virtual implants and help create the foundation for a computer assisted surgical guide. The regenerated bone volume appeared adequate to receive 4.2 x 10.5mm tapered internal implants. These fixtures were placed virtually, and my implant plan was digitally transferred to Simplant to design and produce a SAFEguide for guided surgery. The advantages of implant planning in this manner are twofold, we learn immediately if our previous regeneration treatments were successful and can prepare for the next phase of treatment within the 3D software, giving us the necessary information to facilitate the production of a surgical guide. (figs. 6-8)
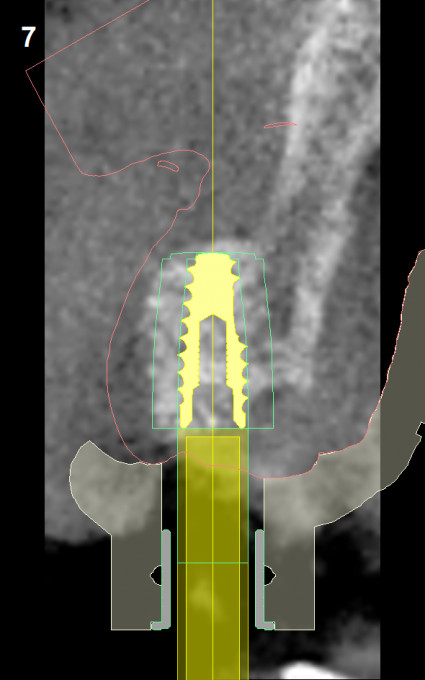
Figure 6: #7 Simplant implant plan with a 4.2x10.5mm implant and surgical guide design
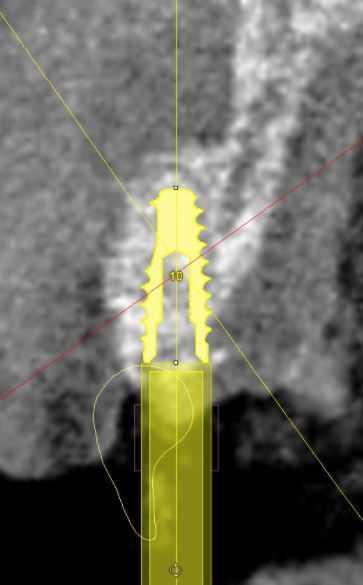
Figure 7: #10 Simplant implant plan with 4.2x10.5mm fixture
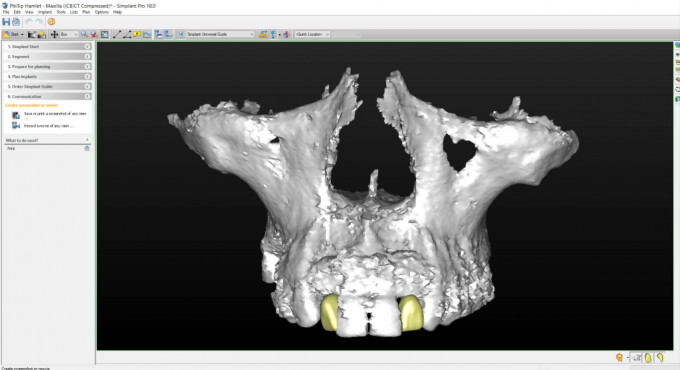
Figure 8: Simplant screenshot of virtual teeth and labial bone augmentation of #7 and 10
Guided Implant Surgery
Our patient was premedicated with amoxicillin 500mg in preparation for his implant surgery. There are studies that have shown this regimen lessens early implant failures. The surgical sites were anesthetized with 4% Articaine with 1/100,00 epinephrine. The SAFEguide tooth borne surgical guide was well fitting and stable. We gained a good volume of bone which was accessed through mini flaps. The osteotomies for # 7 and # 10 were prepared through the guide. I noted that the bone was soft, D3 D4 in density but the implants were torqued in sufficiently to gain stability, a pre-requisite for Osseo-integration. I anticipated uncovering the 4.2 x 10.5 mm tapered implants after 12 weeks. Upon follow up I obtained an updated cone beam and discovered apical fenestrations, so I accessed these areas via trapezoidal flaps and added additional bone to both sites. This unexpected complication set the restorative phase of treatment back a couple of months, but the results were favorable after 6 weeks verified with 3D imaging. The cross-sectional views show improved apical coverage of both implants and the tissue appeared healthy. (figs. 9-13)
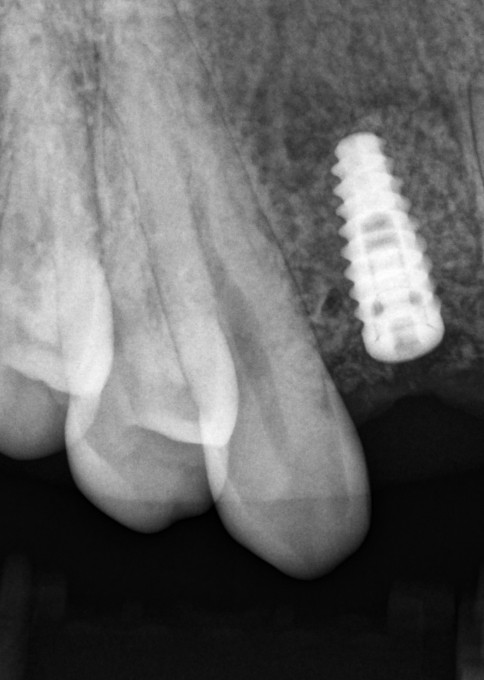
Figure 9: 4.2x10.5mm tapered implant #7
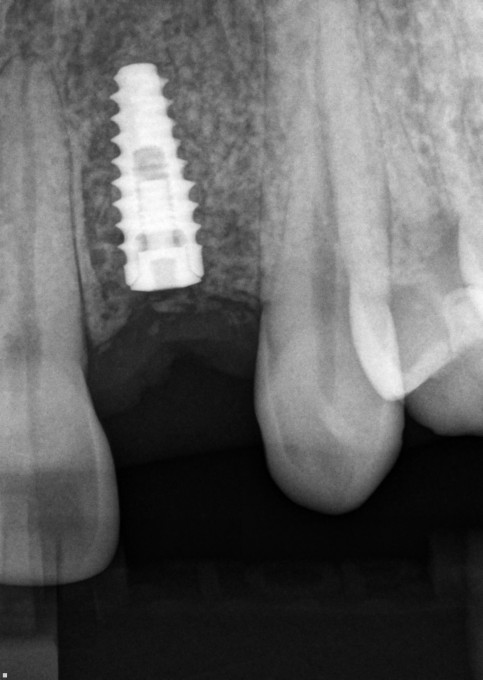
Figure 10: 4.2x10.5mm tapered implant #10

Figure 11: Post-op revised bone graft implant #10

Figure 12: #7 xsectional Sidexis 3D view post bone regeneration prior to restoring

Figure 13: #10 xsectional Sidexis 3D view post bone regeneration prior to restoring
Restorative Workflow
Uncovering was performed through tissue punch access through the surgical guide. I temporized with PEEK prefabricated abutments and Luxatemp crowns. A printed model with acrylic denture teeth replaced #s 7 and 10 which was used to create an omnivac shell as a blueprint for the provisionals. Osstell ISQ values were obtained indicating high stability (any value 70 or higher) and provided objective confirmation that these implants were ready to be restored. Osstell ISQ values are taken at different times to determine when the implants were biologically stable and provides supporting documentation for our clinical decision to move forward with the restorative phase of treatment. The results were good, and the final optical impression would be obtained after the gingival tissue healed and our emergence profile could be optimally managed. (figs. 14-18)
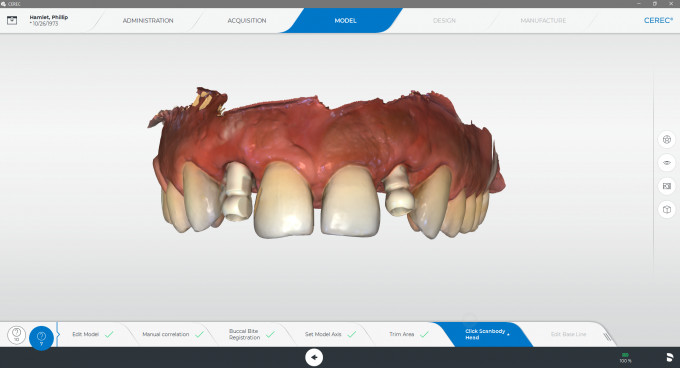
Figure 14: Primescan optical impression of site specific IO Flo scan bodies capturing fixture level impression
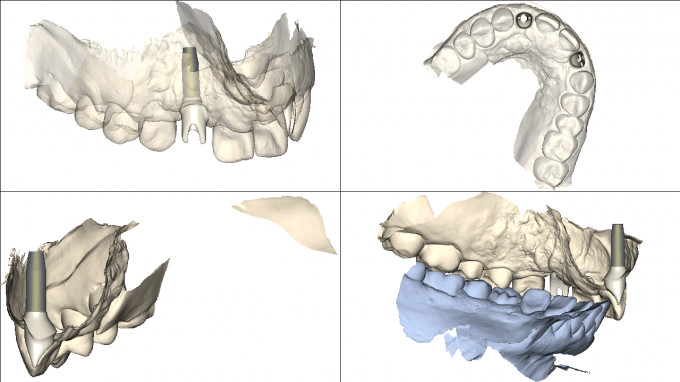
Figure 15: Atlantis design reviewed and accepted
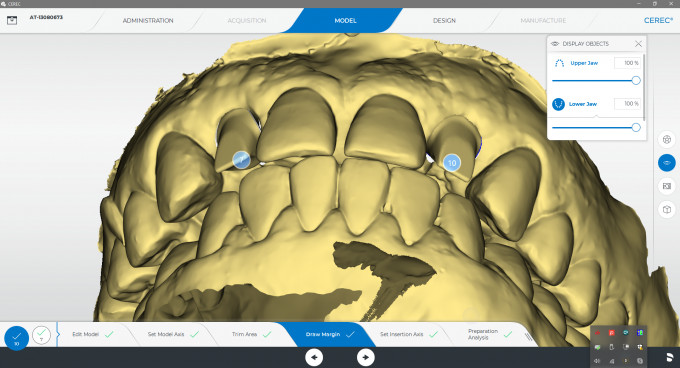
Figure 16: Model phase derived from Atlantis .dxd core file used to design and manufacture e.max crowns
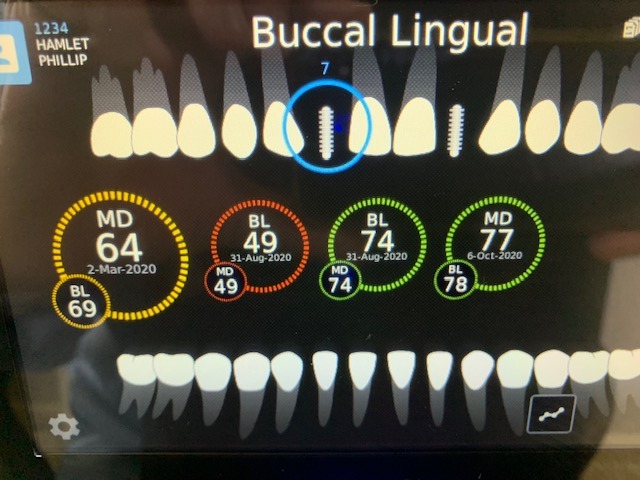
Figure 17: Osstell ISQ values for # 7 Implant indicating successful osseo-integration. Note the 49 value was caused by bone interfering with the digital reading, revalued at 74 same visit
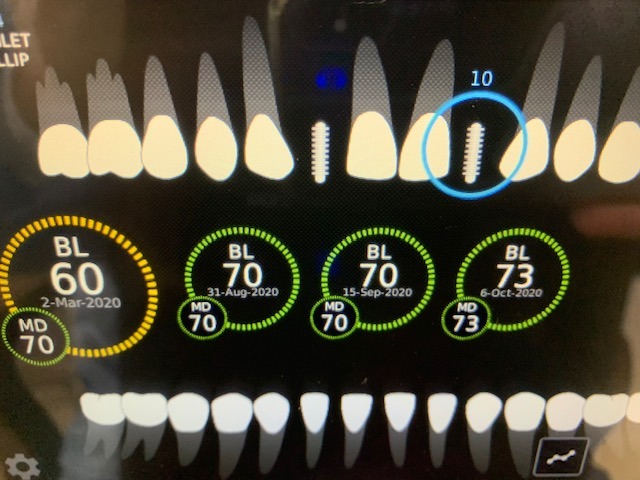
Figure 18: Osstell ISQ values for # 10 implant indicating successful ooseo-integration
The CEREC digital workflow to fabricate Atlantis abutments is, in my opinion, the ideal way to produce CAD/CAM custom abutments that are efficient, productive, functional and economical. The manufacture of a screw-retained or cementable implant crown and Atlantis abutments comes with a significant cost savings. Routinely a 25-40% reduction in cost as compared to the dental lab. In addition, I can review the design and make any necessary changes to achieve an optimal outcome. This case is illustrative of such a restorative outcome. An optical scan of the site-specific IO Flo scan body for the implant was captured and digitally transferred through the CEREC Connect Case Center to the Atlantis lab. A materials reference guide is available for the clinician to review and decide which abutment is appropriate for a particular implant site. I chose to utilize a zirconia abutment and selected shade 20 used for midrange shades in the VITA shade guide, i.e. A2. At least 1.5mm of occlusal clearance and 1 mm of axial wall depth provides adequate space for restorative strength. The gingival chamfer margins would be placed .5mm subgingivally in the labial, mesial and distal positions. The lingual margin would be at the gingival crest. The cement margins would be easy to clean at the insertion visit by placing the margins at these levels. I requested a core file which was downloaded into CEREC before the Atlantis abutment was delivered to my office and used for the design and manufacture of the e.max crowns. These restorations are milled, stained and glazed by my assistant before the abutments arrive at the office, usually a two-day turnaround. Much faster than the local lab turnaround times. The Atlantis lab always includes an insertion jig with these kinds of abutments to make the insertion visit a non-event. An accurate Primescan impression is key to capture the IO Flo scan bodies seated into the implant registering the correct implant position in situ. Both abutments were torqued in to 30 ncm and their access holes covered with Teflon tape and resin. The abutments were seated with little effort and the e.max crowns were cemented onto the abutments completing the restorative phase of treatment. A slight reduction in the uneven incisal edge on # 8 was the final enhancement to this case. The CEREC digital workflow facilitates this restorative process to a point where no occlusal adjustments were necessary during the insertion visit. Implant protected occlusion is built into the occlusion to avoid any physiological overload of masticatory forces during function. Esthetic and functionally demanding cases can easily be incorporated into our CEREC chairside workflow with these approaches. The optical properties of e.max are consistent and when the proper block shade and translucency is selected, these lithium disilicate ceramics produce a natural, esthetic, well-fitting and biocompatible restoration. (figs. 19-22)

Figure 19: Peri-implant tissue at restorative visit

Figure 20: e.max crowns completed and fitted prior to insertion visit

Figure 21: Zirconia abutments and e.max crowns

Figure 22: Insertion jig during installation of # 10 zirconia Atlantis abutment
Success is determined by clinical and radiographic post loading evaluations. The patient was seen two months after his restorative visit and remarked that he loved the look and feel of his new teeth. Success will include healthy keratinized gingival tissue, no bleeding upon probing and minimal sulcular depths. His surgery maintained all papillae which added to the natural looking esthetic result. The use of zirconia Atlantis abutments enhanced the e.max crown which reflected light as well as his adjacent natural dentition. It is important to monitor the crestal bone levels over time which should exhibit minimal or zero bone remodeling ensuring a healthy and optimally functioning dental implant. (figs. 23-29)

Figure 23: #10 zirconia Atlantis abutment

Figure 24: Right side view post op loading

Figure 25: Left side view post op loading
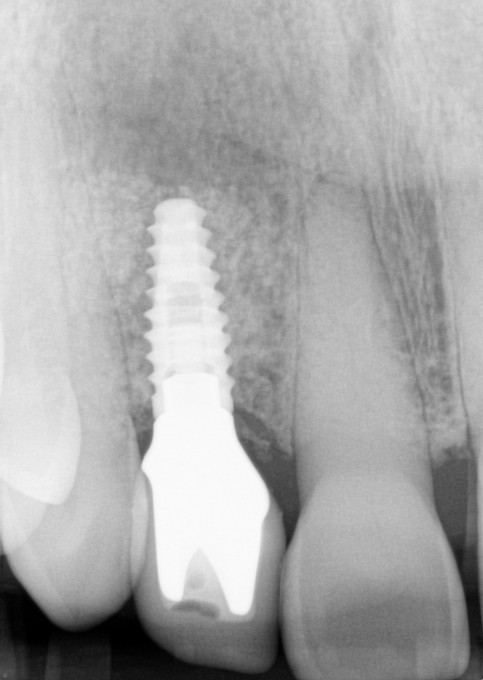
Figure 26: Definitive emax implant crown # 7 cemented onto Zirconia Atlantis abutment
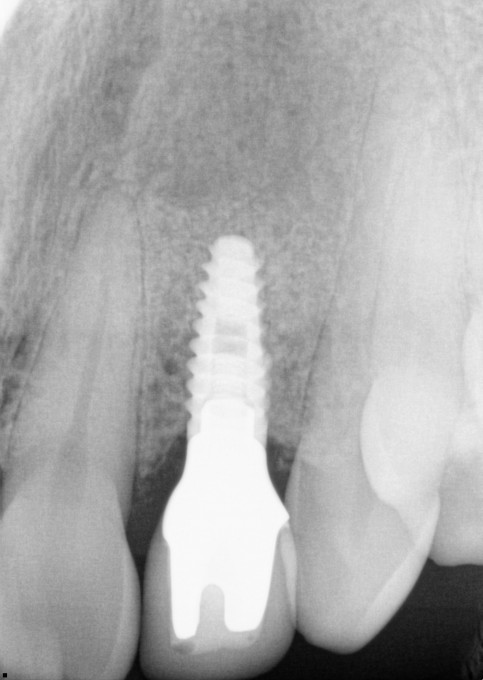
Figure 27: Definitive e.max implant crown # 10 cemented onto Zirconia Atlantis abutment

Figure 28: Completed e.max restorations
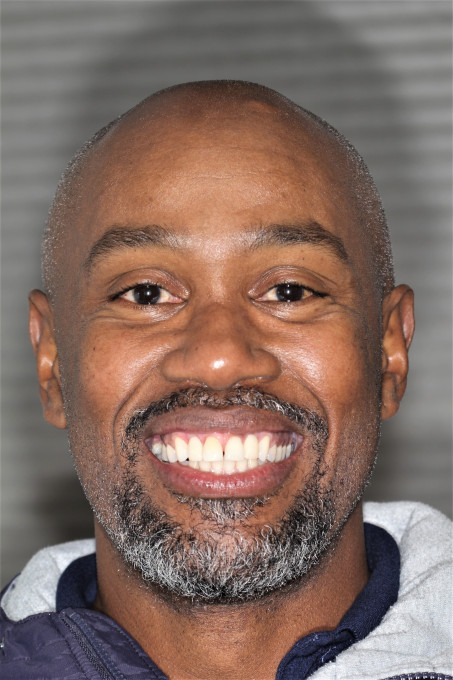
Figure 29: A happy confident smile
Control of the Process Leads to Success
Only with a full understanding of the challenges associated with these complex cases can a viable solution be planned and executed to our satisfaction. Preparing to succeed before any treatment is performed with advanced 3-dimensional implant planning, a direct benefit of our in-office digital technologies. Being in control of all the processes to treat both the surgical and restorative phase of implant dentistry has been a practice builder leading to securing case acceptance during our patient's initial visit. Technology goes hand in hand with clinical skills to empower the clinical side of the practice by opening new avenues for expanded services. The goal is to replace missing teeth in a safe, predictable and streamlined approach while providing long lasting solutions. In this case, replacing two missing teeth with fixed tooth replacements changed our patient's life. His priceless smile displays a newfound confidence, derived from both functionality and esthetic appearance, that will serve him throughout his life. Note how the light is reflected off both his natural teeth and restorations to provide a natural blended appearance. A predetermined game plan preceded our efforts to improve the foundation for implants and precipitated a straightforward restorative case
Nice case and nicely documented. My only comment, and this is based only on my experience, is that all zirconia abutments have not held up to occlusal stresses very well, and the fragments when they break can be a pain to remove.
On 5/5/2021 at 4:55 pm, Gary Templeman said...Nice case and nicely documented. My only comment, and this is based only on my experience, is that all zirconia abutments have not held up to occlusal stresses very well, and the fragments when they break can be a pain to remove.
Gary,
I agree with this comment completely. I stopped using them 6-7 years ago and the industry as a whole has mostly gotten away from them as well. Atlantis still provides them but guaranties them only for 5 years vs. a life time guaranty for their other abutments. In addition to the fracture you noted there is also a study (by Tom Taylor, UCONN) showing that the zirconia actually wears the titanium inside of the implants as it a harder.
Farhad